How To Keep Having Good Sex During Menopause
Ah, sex after menopause—the time in a women’s life that we all finally envision enjoyable intercourse without pain, bleeding, or a fear of getting pregnant. Right? Yes and No. While menopause can and should be one of the most sexually liberating periods in a woman’s life, it’s perfectly normal that it may take time to adjust for some. Vaginal dryness, thinning, and atrophy are just a few examples of how diminishing estrogen levels may present new challenges in the bedroom.
During our 20s, 30s, and even well into our 40s our vaginal lining has plenty of estrogen, making it thicker and more flexible, allowing for both comfortable and enjoyable sex as well as ease of having children.1 Starting during perimenopause, estrogen levels begin to decrease, which also coincides with a decrease in vaginal thickness and elasticity.1
This can lead to painful sex, but even worse, it can cause tearing, injury, and even bleeding, making intercourse miserable at best.1 On top of it all, lower estrogen levels can decrease libido beginning in perimenopause, and cause mood swings, which can lead to further stress as well.2 Common menopausal symptoms unrelated to sex, such as night sweats, can disrupt our sleep cycle leaving us too exhausted to consider intimacy.2
These complications, however, shouldn’t deter us from embracing the sexual freedom menopause should bring. If anything, symptoms such as these should be a reason to perk up, listen to your body, and seek a solution to feeling good again, in and out of the bedroom. Two out of three women retain both sexual interest and satisfaction through the menopausal transition.3
Check out our tips below:
Consider this option for menopause symptom relief†
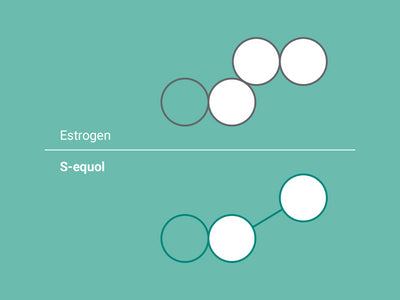
Now, there’s an effective, non-hormonal‡ option available to alleviate menopausal symptoms: only EQUELLE offers the active ingredient, S-equol, to provide real relief. S-equol has a similar structure to estrogen and can mimic some of its actions, helping to ease menopause symptoms. S-equol is naturally-derived, plant-based and has been shown to be safe to use. EQUELLE has been clinically validated to reduce the frequency of hot flashes, support the quality of sleep, alleviate mood swings, and reduce vaginal irritation, soreness, and itching.†§ 92% of patients were satisfied with EQUELLE after a 12-week trial and with a 60-day money-back guarantee, you can try it risk-free. Click here for more details
Define what “good sex” means to you
Discovering what works for you during menopause may take some exploring and a little imagination. Trying new positions with your partner may be one way to see what you can do to get your heart pumping for all the right reasons. If there’s ever been a time to make sure our needs are met, it’s now. It’s not time to be shy.
Do something active every day
When it comes to having a good time between the sheets, it never hurts to build up your cardio and strengthen your muscles to improve stamina. In addition, regular exercise can boost your energy level and mood as well.2
Communicate with your partner
Honest conversations with your partner can help make this transition smoother and might even create a stronger bond between you, and a platform for creativity. Be open about which positions you like, what feels good and what doesn’t, and how much time you need to get aroused. Menopause is a great excuse to explore new ways of being intimate.
Continue to practice safe sex
Using protection is important during perimenopause to prevent pregnancy and remains important after menopause as well if you are not in a monogamous relationship. Vaginal dryness and irritation can lead to small cuts or tears during sex, which makes it easier to contract an STD.2 Even if you can’t get pregnant anymore, condoms do help prevent STDs as you explore your sexuality.
Try some lubricants or moisturizers
Water-based lubricants or vaginal moisturizers are both safe options for giving your V the extra support it needs during any stage of life—but especially menopause when a lack of estrogen can lead to a thinner and drier vaginal lining.
Have even more sex
A lack of estrogen can cause our vaginal tissues to tighten, dry, and thin—making sex uncomfortable.2 Drier tissues are more prone to tearing and bleeding during penetration, which can be painful even with a lubricant.2 Believe it or not, regular sexual activity can help keep your tissues healthy, by increasing blood flow to the vagina.1
Make time for foreplay
Allowing yourself the time it takes to get properly aroused, naturally helps your body by providing moisture that protects tissues and helps make sex more enjoyable. 2
Try some pelvic floor exercises
Strengthening the muscles you need to orgasm can help to increase blood flow to the vagina. Improved circulation and blood flow to all of the tissues in the pelvis goes a long way during intercourse!2
Avoid drugs, alcohol, and smoking cigarettes
Drugs and alcohol can slow down your body’s response systems. Smoking cigarettes actually lowers the body’s estrogenic effects which can further reduce blood flow to the vagina, making it difficult to get aroused.2
Avoid products that irritate your vagina
Who doesn’t love a nice long soak in the bathtub after a long day? Just make sure your bath bombs and bubbles aren’t causing any unnecessary irritation or itching.
Talk to your doctor
There might be products like pills or creams that can help with treating lower female sex drive. Your doctor may be able to prescribe other options as well such as vaginal creams, tablets, or rings with estrogen. Even if you choose not to use any of these options, it’s a good idea to keep regular appointments with your doctor to check in about any changes you may be experiencing during menopause—whether or not they’re related to your sex life.
Plan your intimate getaway
Trying to squeeze sex in during a stressed and busy day may not be right for what your body needs. Sometimes part of the ritual is being thoughtful about timing, allowing for enough time needed to properly prepare for and enjoy sex. Plan a romantic weekend getaway or listen to your body’s signals during the week. You may find you’re more receptive to intimacy once you’ve crossed a few things off your to-do list. Make time for yourself and your partner.
Try a hormone-free, naturally-derived supplement to provide symptom relief
There are non-hormonal options available to provide relief of symptoms of vaginal discomfort! EQUELLE is a twice-a-day supplement with the active ingredient, S-equol, which is naturally-derived and plant-based. S-equol has a similar structure as estrogen and can mimic some of its actions, helping to ease menopause symptoms. EQUELLE has been clinically validated to reduce vaginal irritation, soreness, and itching†§ 92% of patients were satisfied with EQUELLE after a 12-week trial and with a 60-day money-back guarantee, you can try it risk-free. Click here for more details.
Remember sex is meant to be fun!
Losing interest in sex as we age isn’t a medical condition that needs treatment. If you’re happy with the changes menopause has brought to your bedroom, then live on! Stick with whatever works for you, and don’t push yourself too much. Getting to know your new sexual needs during menopause is much like sex itself—we may need a little warming up before we find our stride.
This information is only for educational purposes and is not medical advice or intended as a recommendation of any specific products. Consult your health care provider for more information.
References
- The North American Menopause Society. “Changes in the Vagina and Vulva.” 2019. Accessed on: December 2, 2019. <https://www.menopause.org/for-women/sexual-health-menopause-online/changes-at-midlife/changes-in-the-vagina-and-vulva>
- US Department of Health & Human Services. “Menopause and sexuality.” 2018. Office of Women’s Health. Accessed on: December 2, 2019. <https://www.womenshealth.gov/menopause/menopause-and-sexuality>
- Basel, K et al. “Sexuality During Menopause.” The Menopausal Transition. Soares, CN, Warren, M. 2009. 18–40.